Ultrasound Course Module 5
Biometry, Prenatal Diagnosis, and Doppler
Lesson 4: Doppler/Color Flow
- Doppler first noted by Christian Doppler in the 19th century. Pitch of sound of a moving object is changed when the distance between the observer and the source of the sound changes. This change caused by the relative motion between an observer and the object is the Doppler shift. As a consequence, when the sound emitted from a stationary source is fixed and the angle of the sound is known, the Doppler shift (difference between the emitted and the reflecting frequency) can be calculated, since it is correlated to the velocity of the relative movement between the target and the transducer. The formula is:
Doppler shift = 2 (frequency of transmitted sound) x (velocity of relative movement) x (cosine of angle of insonation/velocity of sound in the tissue)
-
 Normal pulsed Doppler for
Normal pulsed Doppler for
valvular rhythm and function
Continuous Wave (CW) Doppler utilizes separate emitting and receiving transducers set up so that the axes intersect at a certain range determined separately for each pair of transducers. They operate continuously and therefore are not limited by a maximum detectable velocity range. All Doppler signals originating from a certain range of the area are all superimposed making actual visualization of vessels impossible. (Gill RW. Doppler ultrasound: physical aspects. Semin Perinatol 1987;11:292-99.)
- Pulsed Doppler uses ultrasound emitted in a pulsatile fashion. Between pulses of emission, the same transducer operates as a receiver for the back-scattered echoes. Since the velocity is known and thought to be constant, it is possible to analyze the back-scattered echo alone from a particular range. A circuit selectively allows only those signals that arrive to the receiver at a specific time after the transmission. This allows a precise determination of the size of the sample volume that can be located in a specific area. (Gill RW. Doppler ultrasound: physical aspects. Semin Perinatol 1987;11:292-99) The sequence of transmit-and-receive is repeated periodically. The rate at which this is accomplished determines the performance of the pulsed Doppler system.
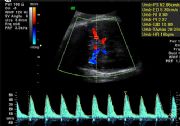
 Color flow Doppler of fetal
Color flow Doppler of fetal
heart to show cross over of
Left Ventricular Outflow Tract
(LVOT) and Right Ventricular
Outflow Tract (RVOT)
- The biggest problem of pulsed Doppler is the limit that a new pulse cannot be emitted before the last echo of the preceding pulse has arrived at the transducer.
- The maximum Doppler shift frequency that can be measured is equal to half the pulse repetition frequency (Nyquist limit). After this, the Doppler is distorted (aliasing). This may be solved by increasing the pulse repetition frequency or lowering the baseline. This may occur in color Doppler imaging.
- Real-time ultrasound and pulsed Doppler is called duplex Doppler scanning. This combines real-time imaging with the Doppler.
- Color Doppler uses color-coded pulse Doppler on top of the B-mode ultrasound image. Color is usually assigned a direction. Usually blood flow toward the transducer is red and blue color is flow away from the transducer. Color saturation is relation to the magnitude of the frequency shift. (Carroll BA, von Ramm OT. Fundamentals of current Doppler technology. Ultrasound Q 1988;6:275) This allows the detection of small vessels and slower blood-flow velocity. Color flow imaging has the same limitations as pulsed Doppler.
- Color Doppler energy (CDE) detects energy of Doppler signals from moving blood. It is independent of blood flow. This enables detection of low flow. Pulsed wave Doppler uses the total spectral content of Doppler signal within a single sample volume. Conventional color Doppler imaging displays 2 parameters of the Doppler signal: variance (width) and mean velocity. They are both given colors to display on the monitor. CDE displays the third parameter of strength or energy.
- Difference between CDE and the usual color Doppler imaging (CDI) may be noted as:
- CDE is not dependent on the mean velocity but on amplitude and is therefore angle independent.
- CDE is displayed over lower volumes and velocities.
- CDE is not affected by aliasing.
- Allows better investigation of blood flows at lower velocities and at angles even consistent with 90 degrees of insonation.
- Doppler Velocimetry usually allows the measurement of Doppler shift of only one frequency.
- Doppler signals detected by the receiving transducer are a mixture of different Doppler shift frequencies. This mixture of frequencies is analyzed by an on-line computer and transformed into a series of spectra (Doppler spectrum) that are graphically displayed in real-time.
- These representations (flow velocity waveforms) show the relative power of each frequency component that constitutes the entire Doppler signal.
- The mean flow velocity waveform (FVW) is related to three variables: time, frequency, and power. The power of the frequencies reflects the volume of blood moving at a certain velocity. The power is represented as brightness of the spectrum.
- Quantitative Analysis depends upon the Doppler frequency shift and angle of the insonation. The Doppler shift frequency decreases toward 0 as the insonation angle approaches 90 degrees (i.e., cosine=90, degrees=0). Doppler measurements are reliable as long as they are interrogated at an angle < 60 degrees. As an example, at 60 degrees, a 2-degree error in the angle would result in a 6% error in Doppler shift estimation. (Dickerson KS, Vernon MS, Newhouse VL, et al. Comparison of conventional and transverse Doppler sonograms. J Ultrasound Med 1993;12:497-506)
- Semiquantitative Analysis allows for use of the ratio between the systolic and diastolic ratios to correct for the angle of insonation. The ratio negates the need to be concerned with the angle of the ultrasound beam or its error related to the angle. The most common equations include:
Pulsatility Index (PI) = S (maximum peak systolic frequency) - D (end-diastolic) / A (mean Doppler shift frequency)
PI=S-D/A
Resistance Index (RI)= S-D/S
The indices are well correlated to outcomes. (Thompson RS. Blood flow velocity waveforms. Semin Perinatol 1987;11:300-310) The PI and RI reflect the downstream flow impedance. These are affected most by the compliance of the vessels in the system. Therefore, vasodilation causes a decrease in impedance and vasoconstriction causes an increase in impedance. Doppler shifts in this system depend on blood-flow type, the size of the sample volume, insonation angle, vessel type, and depth of the target.
- Safety in ultrasound has long been established but specific biologic effects ought to be explained. (Kieler H, Axelson O, Haglund B, et al. Routine ultrasound screening in pregnancy and the children's subsequent handedness. Early Hum Dev 1998;50:233-45. & Salvesen KA, Vatten LJ, Iik-Nes S, et al. Routine sonography in utero and subsequent handedness and neurological development. Br Med J 1993;307:159-64. & Lyons EA. Human epidemiological studies. Ultrasound Med Biol 1986;12:689. & Newnham JP, Evans SF, Michael CA, et al. Effects of frequent ultrasound during pregnancy: A randomized controlled trial. Lancet 1993;342:887-93)
- Acoustic Power represents the amount of energy produced per unit of time: relates to duration of pulse, the pulse repetition frequency (reciprocal of interval between pulses), and the duty factor (the pulse duration divided by the pulse repetition frequency). This is related specifically:
I (intensity) = Power (watts/area in cm2)
- Thermal effects or tissue heating depends on ultrasound frequency, intensity, the area of the ultrasound beam, and exposure time. Tissue type also affects the heat absorption (bone/soft tissue absorb more heat). Broader beams produce more heat. In the usual diagnostic ultrasound the rise in temperature does not exceed 1 degree Centigrade when the ISATA (spatial average, temporal average intensity) stays below 300 mW/cm. Biologic effects may occur above 39 degrees Centigrade. A temperature rise of 2 degrees Centigrade in an afebrile patient will not cause any harm unless the time limit is exceeded. The World Federation of Ultrasound in Medicine and Biology notes "any in situ temperature rise to or above 41 degrees Centrigrade for 15 minutes should be considered hazardous in embryonic and fetal exposures; the longer this temperature is maintained, the greater the likelihood for damage to occur." (Merritt CRB, Kremkau FW, Hobbins JC. Diagnostic ultrasound: Bioeffects and safety. Ultrasound Obstet Gynecol 1992;2:366-74)
- Mechanical effects are more subtle with cavitation as the result with high power. This only happens with intensities greater than 1.5 MPa.
- Thermal index (TI) and mechanical index (MI) were developed to measure ultrasound effects. The thermal index is defined as the ratio of acoustic power in mW to the power necessary to heat a particular tissue by 1 degree Centigrade. This gives an estimate of the tissue temperature rise in degrees centigrade under worst case scenarios. There are three types of thermal indices: soft-tissue index (TIS) and two bone indices (TIB and TIC). TIB measures temperature where bone is located near focus of the beam and TIC (Cranial Thermal Index) measures the rise of temperature where the scanner is near bone. All scans should be done on the As-Low-As-Reasonably-Achievable (ALARA) principle.
- First trimester Doppler — Doppler has not been established as a safe diagnostic modality in the first trimester. Therefore, Soli Deo Gloria MFM, LLC has established a clinical guideline that discourages the use of any Doppler in the first trimester. Fetal viability may be established by the use of the standard real-time ultrasound and documenting visually with either a tape/digital record or documented fetal heart rate.
- Clinical Doppler Ultrasound

 Absent umbilical artery blood
Absent umbilical artery blood
flow in severe growth delay
 Reversed umbilical artery blood
Reversed umbilical artery blood
flow in severe growth delay
 Normal MCA of 52.9 cm seconds
Normal MCA of 52.9 cm seconds
at 32 weeks in a Duffy
sensitized patient
- Uterine Arteries — progress from a low-volume high resistance to a high-volume low resistance system. The artery is measured at the main branch near the cervicocorporal junction. The normal values change with gestation but generally the pulsatility index (PI) is used and anything > 1.5 is considered abnormal. Also, a uterine artery diastolic "notch" early in gestation may predict the onset of preeclampsia.
- Umbilical Arteries — contains 40% of fetal ventricular output in both arteries. Traditionally the systolic flow to diastolic flow or S/D ratio has been used to monitor fetuses at risk. The umbilical Doppler has been particularly useful in managing patients with IUGR, preeclampsia, complicated medical illnesses (diabetes, lupus, etc). (Harrington K, Carpenter RG, Nguyen M, Campbell S. Changes observed in Doppler studies of the fetal circulation in pregnancies complicated by pre-eclampsia or the delivery of a small-for-gestational baby. I. Cross-sectional analysis. Ultrasound Obstet Gynecol 1995;6:19-28. & Pattinson RC, Norman K, Odendaal HJ. The role of Doppler velocimetry in the management of high risk pregnancies. Br J Obstet Gynaecol 1994;101:114-120. & Trudinger BJ, Cook CM, Giles WB, Ng S, Fong E, Connelly A, Wilcox W. Fetal umbilical artery velocity waveforms and subsequent neonatal outcome. Br J Obstet Gynaecol 1991;98:378-84) The ranges are gestationally determined with slightly higher S/D ratios (> 2.5-4.0) in early gestations prior to 24 weeks and the lower S/D ratios ( < 3.0) greater 24 weeks. The absence of end diastolic or reversed end diastolic flow is particularly worrisome. Most believe that the absence or reversed flow in the umbilical artery S/D ratio means a very high risk of stillbirth within 48-72 hours. (Karsdorp VH, Van Vugt JM, van Geijn HP, Kostense PJ, Arduini D, Montenegro N, Todros T. Clinical significance of absent or reversed end diastolic velocity waveforms in umbilical artery. Lancet 1994;344:1664-8 & Kurkinen-Raty M, Kivela A, Jouppila P. The clinical significance of an absent end-diastolic velocity in the umbilical artery detected before the 34th week of pregnancy. Acta Obstet Gynecol Scand 1997;76:398-404)
More recently, the pulsatility index (PI) has been used since it is not affected by the reverse or absence of end-diastolic flow. Reference ranges are used for the 5th and 95th percentiles. (Harrington K, Carpenter RG, Nguyen M, Campbell S. Changes observed in Doppler studies of the fetal circulation in pregnancies complicated by pre-eclampsia or the delivery of a small-for-gestational baby. I. Cross-sectional analysis. Ultrasound Obstet Gynecol 1995;6:19-28.)
- Middle Cerebral Artery (MCA) — This vessel has been used to detect fetal cerebral blood flow for evaluation of IUGR, medical complications (diabetes, lupus), and fetal isoimmunization. It is the easiest of cerebral vessels to identify by color flow with high sensitivity. (Kirkinen P, Muller R, Huch R, Huch A. Blood flow velocity waveforms in human fetal intracranial arteries. Obstet Gynecol 1987;70:617-21 & Woo JS, Liang ST, Lo RL, Chan FY. Middle cerebral artery Doppler flow velocity waveforms. Obstet Gynecol 1987;70:613-16.) The PI of the MCA decreases during the third trimester. Generally the PI ranges from 1.5-2.5 at 22 weeks to approximately 0.8-1.7 at 40 weeks. (Harrington K, Carpenter RG, Nguyen M, Campbell S. Changes observed in Doppler studies of the fetal circulation in pregnancies complicated by pre-eclampsia or the delivery of a small-for-gestational baby. I. Cross-sectional analysis. Ultrasound Obstet Gynecol 1995;6:19-28.) In the IUGR fetus, the mean MCA PI is lower and the mean systolic velocity higher representing a shunting of blood to the head of the fetus to spare the brain.
- Various Vessels — Doppler has been applied to various vessels in the fetus for evaluation of fetal well-being. These include the thoracic aorta, renal, splenic, adrenal, hepatic arteries, atrioventricular flow, pulmonary arteries, ductus arteriosus, coronary blood flow, umbilical vein, ductus venosus, inferior vena cava, hepatic veins, and pulmonary arteries.
- Clinical Doppler Applications
- Preeclampsia — pathology of preeclampsia is related to endothelial cell dysfunction related to poor cellular invasion with related ischemia. (Chappel L, Bewley S. Pre-eclamptic toxaemia: The role of uterine artery Doppler. Br J Obstet Gynaecol 1998;105:379-82) If the poor perfusion is a major part of the development of preeclampsia, then the ability to measure uteroplacental blood flow could be used to screen low-risk populations for the development of preeclampsia. The measurement of high resistance index values with a persistent early diastolic notch demonstrates high impedance and may be used to predict preeclampsia. (Campbell S, Pearce JM, Hackett G, Cohen-Overbeek T, Hernandez C. Qualitative assessment of uteroplacental blood flow: Early screening test for high-risk pregnancies. Obstet Gynecol 1986;68:649-53 & Bewley S, Cooper D, Campbell S. Doppler investigation of uteroplacental blood flow resistance in the second trimester: A screening study for pre-eclampsia and intrauterine growth retardation. Br J Obstet Gynaecol 1991;98:871-79 & Bewley S, Campbell S, Cooper D. Uteroplacental Doppler flow velocity waveforms in the second trimester: A complex circulation. Br J Obstet Gynaecol 1989;96:1040-46)
Various studies have shown sensitivities for prediction of preeclampsia from 25-90%. (Campbell S, Pearce JM, Hackett G, Cohen-Overbeek T, Hernandez C. Qualitative assessment of uteroplacental blood flow: Early screening test for high-risk pregnancies. Obstet Gynecol 1986;68:649-53 & Bewley S, Cooper D, Campbell S. Doppler investigation of uteroplacental blood flow resistance in the second trimester: A screening study for pre-eclampsia and intrauterine growth retardation. Br J Obstet Gynaecol 1991;98:871-79 & North RA, Ferrier C, Long D, Townend K, Kincaid-Smith P. Uterine artery Doppler flow velocity waveforms in the second trimester for the prediction of preeclampsia and fetal growth retardation. Obstet Gynecol 1994;83:378-86)
The most accurate prediction for preeclampsia involves a double notch seen in the uterine artery with a RI greater than the 95% for gestational age at 24 weeks. This gives a positive predictive value of 50% for preeclampsia and 54% for any other complication (IUGR). Further, this will find over 80% of patients with severe preeclampsia requiring delivery prior to 34 weeks. (Harrington K, Cooper D, Lees C, Hecher K, Canpbell S. Doppler ultrasound of the uterine arteries: The importance of bilateral notching in the prediction of pre-eclampsia, placental abruption or delivery of a small-for-gestational-age baby. Ultrasound Obstet Gynecol 1996;7:182-88)
- IUGR — IUGR at the 3rd and 10th percentiles may be predicted at the 20% and 15% with positive predictive values of 12% and 35% with uterine artery RI of greater than the 95th percentile. (Bewley S, Cooper D, Campbell S. Doppler investigation of uteroplacental blood flow resistance in the second trimester: A screening study for pre-eclampsia and intrauterine growth retardation. Br J Obstet Gynaecol 1991;98:871-79.) This information has not been replicated in multiple studies so must be interpreted with caution. S/D ratios also may be used to manage IUGR pregnancies with elevated S/D ratios (> 4), absent end-diastolic flow, or reversed flow predicting significant morbidity and mortality.
-
 Color flow with
Color flow with
absent right artery
 Transverse with only
Transverse with only
one umbilical artery
seen instead of 2
 Vasa Previa
Vasa Previa
Fetal Anemia — The increase in cardiac output has been attributed to the decrease in blood viscosity due to lower hematocrit level during anemia which increases the venous return to the heart and consequently the preload. The peripheral resistance decreases and allows a larger amount of anemic blood flow with less oxygen going to the brain, heart, and adrenal glands. Human studies show blood flow increases in the uterine vein (Iskaros J, Kingdom J, Morrison JJ, Rodeck C. Prospective non-invasive monitoring of pregnancies complicated by red cell alloimmunization. Ultrasound Obstet Gynecol 1998;11:432-37), ductus venosis (Hecher K, Snijders R, Campbell S, Nicolaides K. Fetal venous, arterial, and intracardiac blood flows in red blood cell isoimmunization. Obstet Gynecol 1995;85:122-28) and MCA (Mari G, Adrignolo A, Abuhamad AZ, Pirhonen J, Jones DC, Ludomirsky A, Copel JA. Diagnosis of fetal anemia with Doppler ultrasound in the pregnancy complicated by maternal blood group isoimmunization. Ultrasound Obstet Gynecol 1995;5:400-05)
Most clinicians now use the elevation of the velocity of the blood flow in the MCA to predict fetal anemia and direct further therapy: either cordocentesis or fetal in utero transfusions.
- Post-Term Pregnancy — The reported incidence of post-term pregnancy (> 294 days) is roughly 4%-14% with those exceeding 43 weeks varying from 2%-7%. Studies of the umbilical artery velocimetry S/D ratios have provided conflicting data. Some studies found an absence of end-diastolic flow detected 91% babies with fetal distress. (Pearce JM, McParland PJ. A comparison of Doppler flow velocity waveforms, amniotic fluid columns, and the nonstress test as a means of monitoring post-date pregnancies. Obstet Gynecol 1991;77:204-08) Another study, however, found only a sensitivity of 7% for predicting poor outcomes with an elevated umbilical artery Doppler velocity. (Zimmerman P, Alback T, Koskinen J, Vaalamo P, Tuimala R, Ranta T. Doppler flow velocimetry of the umbilical artery, uteroplacental arteries and fetal middle cerebral artery in prolonged pregnancy. Ultrasound Obstet Gynecol 1995;5:189-97) Some authors have shown that an S/D ratio of 2.4 predicted an abnormal perinatal outcome with a sensitivity of 57.1% and specificity of 77.8%. (Bower S, Schuchter K, Campbell S. Doppler ultrasound screening as part of routine antenatal scanning: Prediction of pre-eclampsia and intrauterine growth retardation. Br J Obstet Gynaecol 1993;100:989-94)
- Single Umbilical Artery — Incidence varies from 0.5-2.5% among healthy newborns. (Thummala MR, Raju TN, Langenberg P. Isolated single umbilical artery anomaly and the risk for congenital malformations: A meta-analysis. J Pediatr Surg 1998;33:580-85)
The incidence is higher in aneuploid fetuses at 9-11%. (Persutte WH, Hobbins J. Single umbilical artery: A clinical enigma in modern prenatal diagnosis. Ultrasound Obstet Gynecol 1995;6:216-29)
The most common way to diagnose this is to do a transverse view at the level of the fetal bladder and document the color flow around the fetal bladder in color flow. Associated anomalies may run as high as 31% with an SUA. (Chow JS, Benson CB, Doubilet PM. Frequency and nature of structural anomalies in fetuses with single umbilical arteries. J Ultrasound Med 1998;17:765-68)
- Vasa Previa — Valuable in diagnosis of a preventable problem. In all pregnancies it is now suggested that the cord insertion site in the placenta be recognized to prevent catastrophic bleeding with either labor or rupture of membranes. Color Doppler has also been used to identify a nuchal cord, cord entanglement, and fluid flow from the trachea, penis, and nasal passages.

